
Even on the 75th anniversary of its foundation, the NHS came under assault from the far-right. This article tackles the claims of its detractors and shows how a team of volunteers has taken the argument to Parliament to defend the NHS – and the UK economy.
The assault on the NHS
When the NHS was founded, it was a central part of the UK’s post-war social contract. Now, it is struggling to perform and there are increasing calls from the far-right for so-called ‘reform,’ which is often a euphemism for further privatisation and introduction of insurance-based funding.
These calls have been led by former Health Secretary Sajid Javid (an avowed follower of Ayn Rand) and Kate Andrews, formerly of the Tufton Street think tank, the IEA, and now the Spectator.
Javid claimed:
“the 75-year-old model of the NHS is unsustainable. And unless it is radically reformed, the principles on which it was founded cannot survive much longer.” He told the Conservative Party conference that “We shouldn’t always go first to the state – what kind of society would that be? Health and Social Care: it begins at home. It should be family first, then the community then the state.”
They are calling, in other words, for a fundamental change to the business model of the NHS – a public service, free at the point of use and funded through progressive taxation.
Responding to the assault
A project supported by the 99% Organisation, Keep Our NHS Public, Every Doctor, the National Health Action Party and others has been examining the extent, if any, to which these arguments have merit. It concluded that they are both factually unfounded and illogical – and that the damage they could do to the health of both the nation and its economy is enormous.
We pulled together a team of volunteers with expertise ranging from NHS management and senior clinical roles through to strategy, economics and financial analysis. This team produced a report, The Rational Policy Maker’s Guide to the NHS, timed to coincide with the anniversary.
The team analysed three questions:
- What works in practice? – When you look around the world at the different systems in place in different countries, which ones actually perform for their citizens?
- What has gone wrong in the UK? – There is no disputing the fact that the NHS is now struggling badly; what is the root cause of that struggle?
- What kind of system would be sustainable into the distant future? – Given that the UK has a growing and ageing population, what strategy is most likely to stand the test of time?
What works in practice?
Of course, healthcare systems are enormously complex and there are many ways to assess their performance. From the point of view of citizens of a country, there are three things we can ask of our healthcare system:
- first of all, we want it to be effective – when we are ill, we want it to deliver high-quality healthcare at least on a par with what citizens of other wealthy countries receive;
- Secondly, we want it to be equitable – the quality of care we receive should not depend on how wealthy we are or how important we are perceived to be; all citizens should have the same right to high quality healthcare;
- And finally, since we are taxpayers, we want it to be efficient. The definition of efficiency is output (quality of care provided) divided by input (principally money) – we should not be spending more than other countries for the same standard of healthcare.
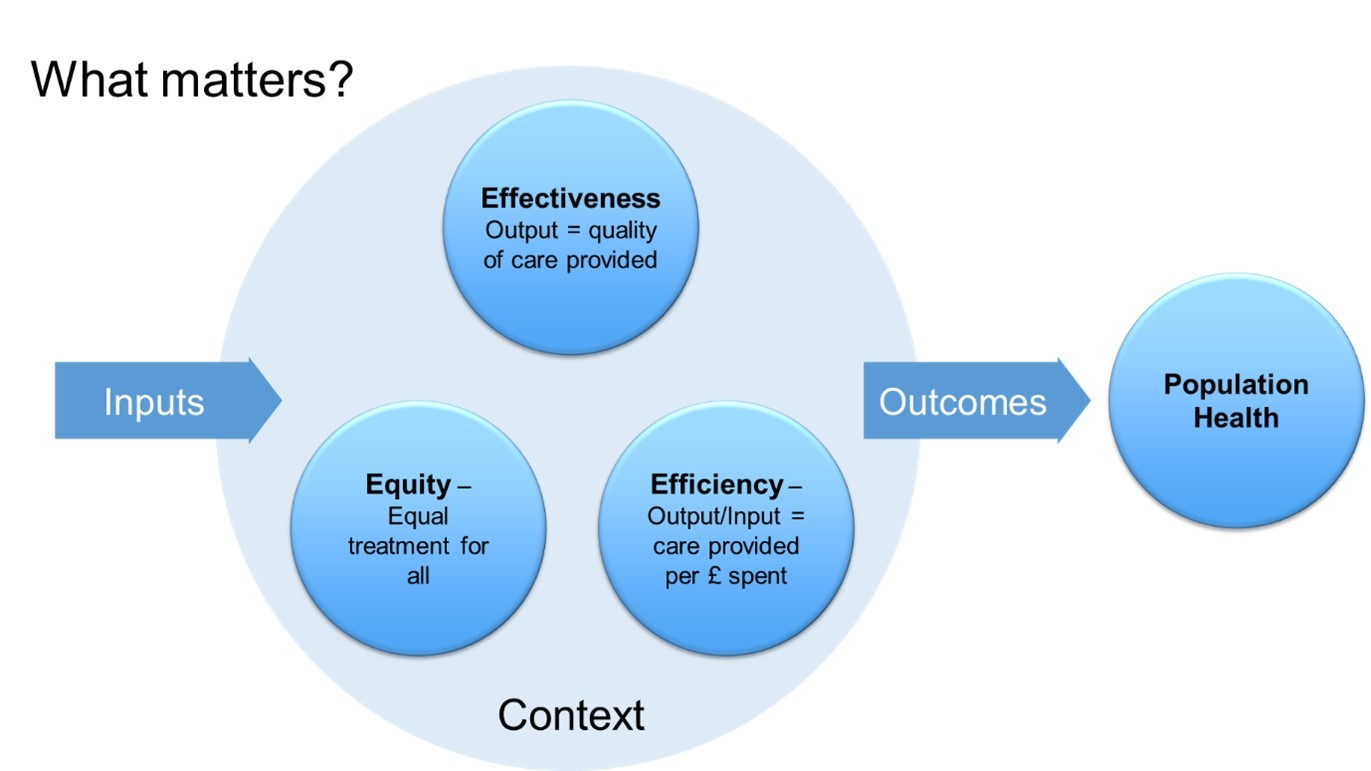
That’s what we can ask, but it is not all we care about. If the inputs are not there, the outputs will be poor. And context matters: the US has very poor life expectancy compared with other countries, and part of that is certainly down to healthcare – but a big part is gun-crime, overdoses, and other ‘external’ causes. Even if the US had the best healthcare system in the world, their outcomes would be poor.
Of the many international benchmarks of healthcare performance, perhaps the most comprehensive are those produced by the Commonwealth Fund. Here is a summary of the Commonwealth Fund’s analysis published in 2014, using data from 2011-2013.
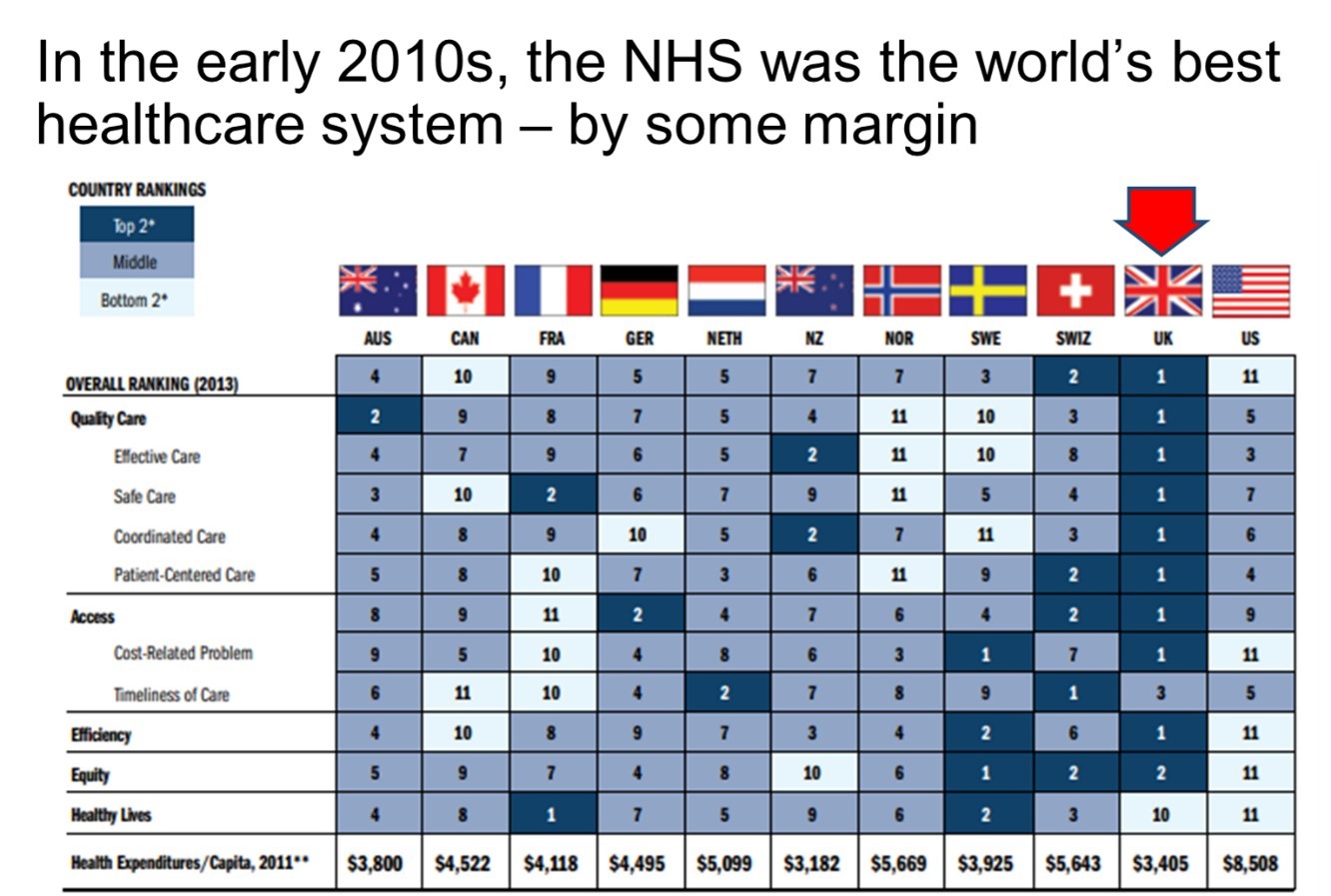
As you can see, the benchmarking shows a clear #1 – the pre-underfunded NHS. Best on outputs – quality of care – best on efficiency, and excellent on equity. Not best on healthy lives because of the context of high levels of UK poverty and inequality.
It also shows a clear #11 – The US system, which is by far the worst in the developed world.
When we look over a longer time we see that the long-term picture is similar. The UK has slipped slightly in recent years and is no longer #1 (though it was still #1 as recently as 2017) – but overall, the UK has the best track record.
This is because the UK system naturally scores very well on equity. A system which is free at the point of use and funded from progressive taxation is the best way of delivering equitable health care.
It also scores extremely well on efficiency – indeed it has often been the most efficient system.
So, in summary, looking around the world to see what works in practice gives a clear answer: the pre-underfunded NHS is the best model so far demonstrated in an advanced economy.
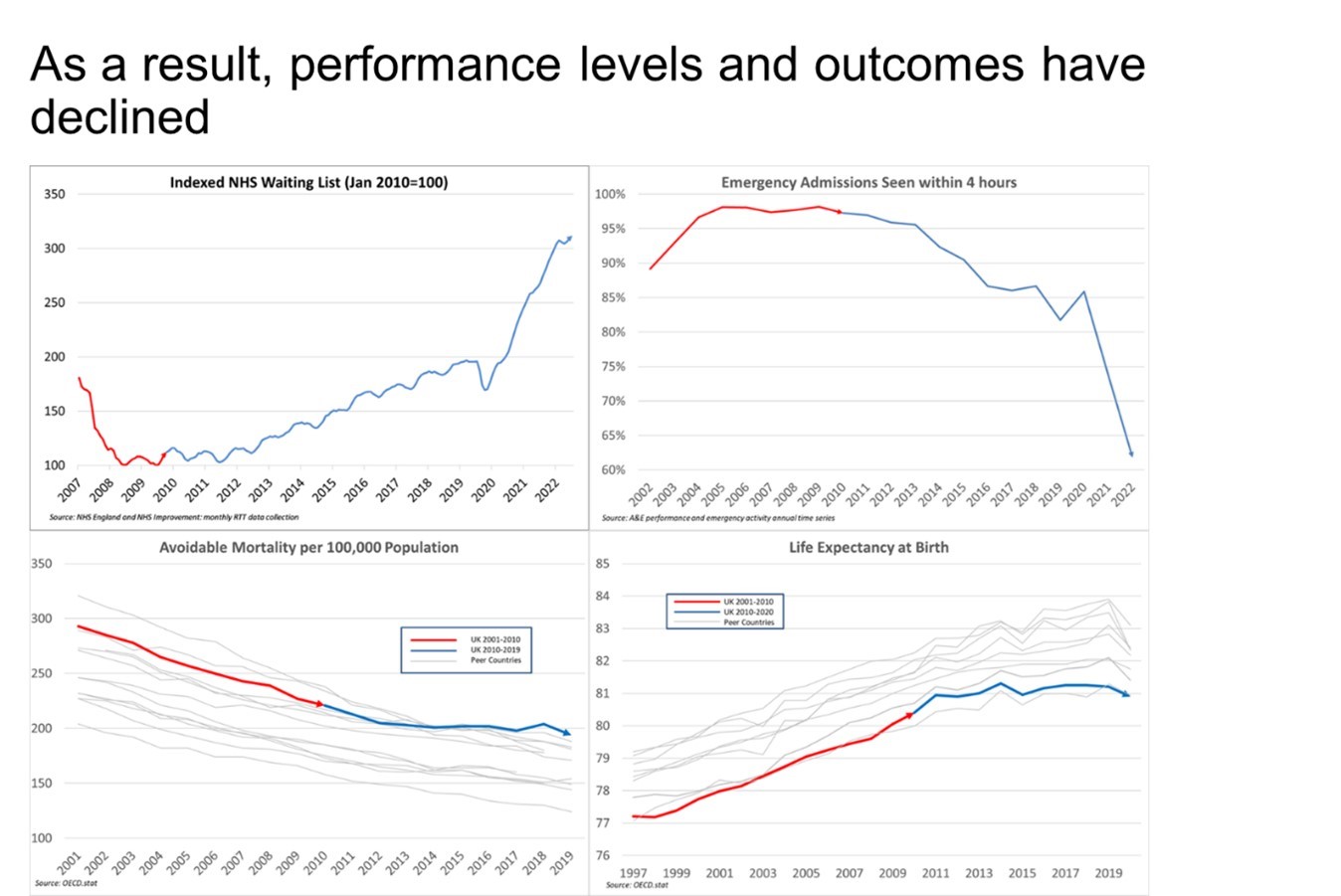
But it is clear that the NHS is struggling today.
What went wrong?
In essence, the answer is simple: underfunding. Since 2010, we have been spending less than other advanced countries, spending a declining percentage of GDP on healthcare, and – most importantly – not keeping pace with the needs of the UK population.
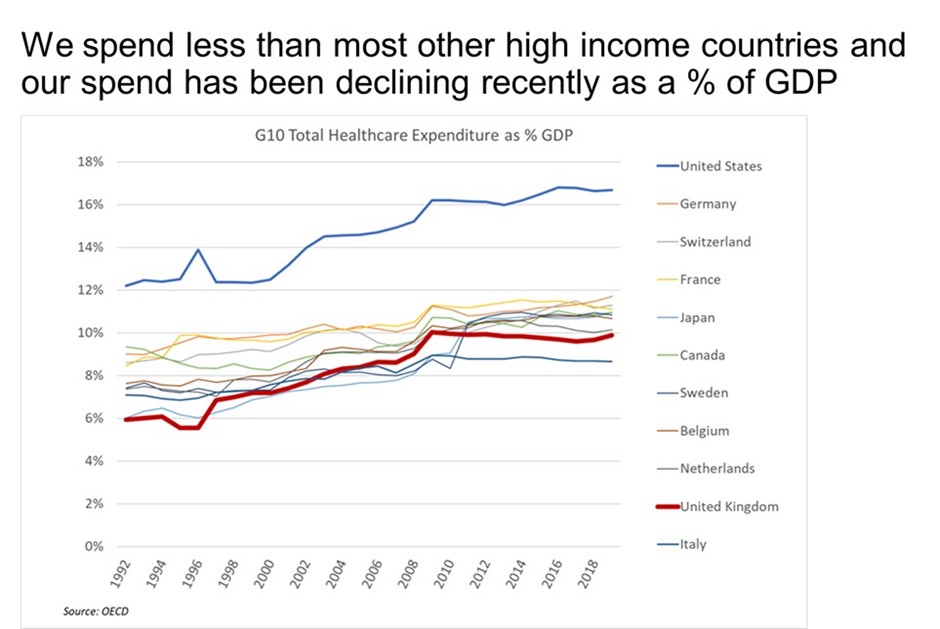
There was a noticeable change in funding policy from 2010 onwards. Before then, as with other countries, the UK had been spending a gradually increasing percentage of GDP on healthcare; since 2010 it has been a gradually decreasing percentage, and spending in the UK is now below almost all other advanced economies.
The result was inevitable: we now have fewer doctors and nurses and fewer hospital beds than almost all our peers, and the service levels we experience have dropped dramatically. The NHS is no longer performing as a world-class healthcare system – and this is directly attributable to the impact of 13 years of underfunding.
No healthcare system in the world could withstand such sustained underfunding.
So, a rational policy maker would have established both that the pre-underfunded NHS was the best model so far demonstrated in an advanced economy and that its underperformance in recent years is due to underfunding. On that basis alone, he or she might be tempted to conclude that the best strategy was to recommit to the fundamental business model over the NHS and to fund it properly.
But what about long term sustainability?
The NHS’s detractors make another unfounded and illogical claim: that with an aging population, funding the NHS will no longer be affordable; we have no option but to change to a different model.
The claim is unfounded because combining the Office for Budget Responsibility data on health spending by age and the Office for National Statistics population forecasts shows no such issue.
It is illogical because if the NHS, the most cost-effective system in the developed world, is unaffordable, then any proven system is unaffordable. A change to an alternative model would bring either much higher spending or much worse health outcomes or, like the US system, a combination of the two.
It is the current government’s policy of underspending which is unaffordable. The reason is simple: the economy is driven by people – specifically healthy people of working age. We currently have around 2.5 million working age adults unable to work due to ill-health; that’s 7% of the total, and rising fast. It is that trend which is unsustainable.
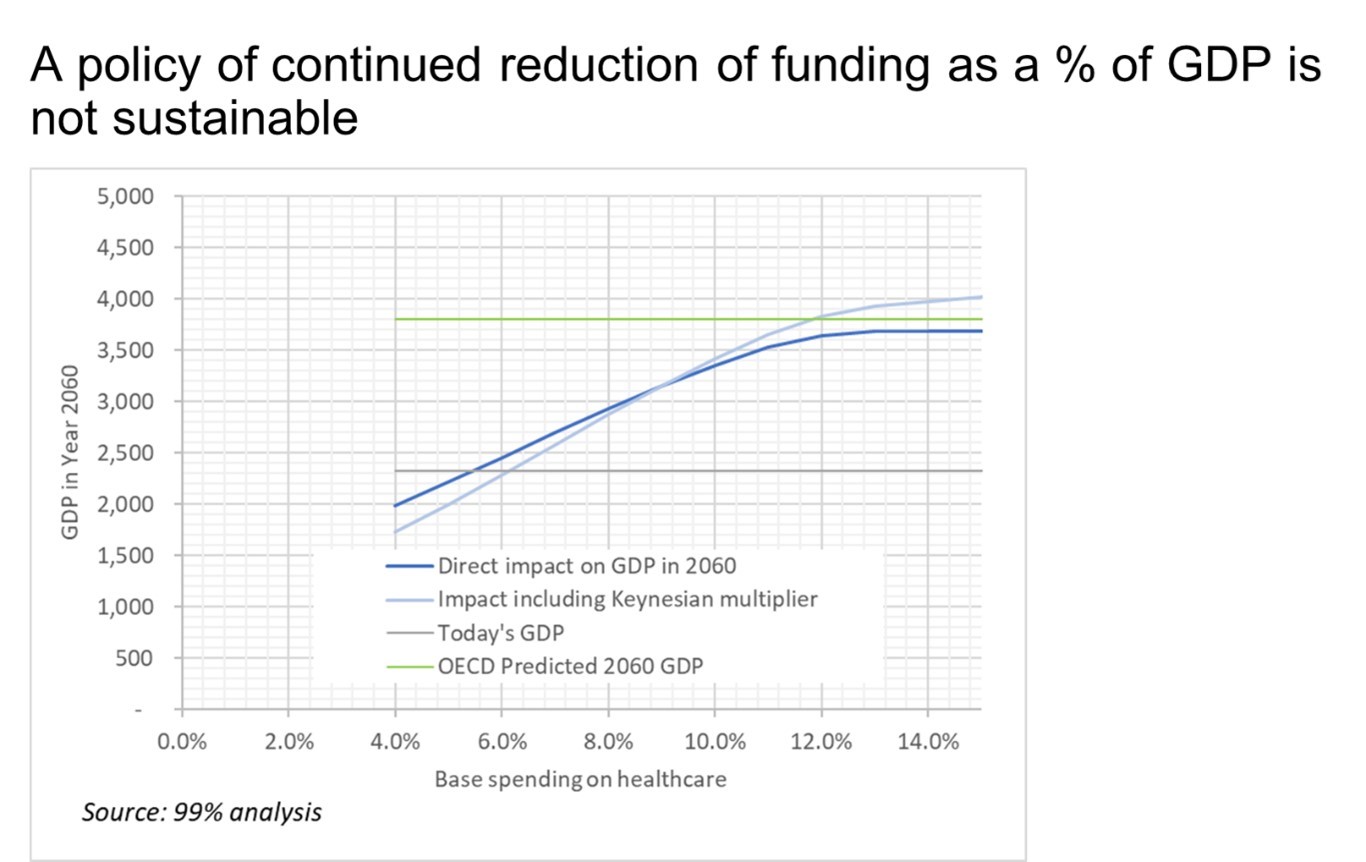
Our analysis shows that if the NHS fails, the economy will fail with it.
The OECD long-term growth forecasts show that by the year 2060, the UK should expect to have a GDP of around £3.8 trillion (vs around £2.2 trillion today); current government health policies would cause a result far worse than the OECD forecasts – they would be economically ruinous for the UK.
A rational policy, adjusting healthcare spending to meet population needs, would produce a spending profile of this form.
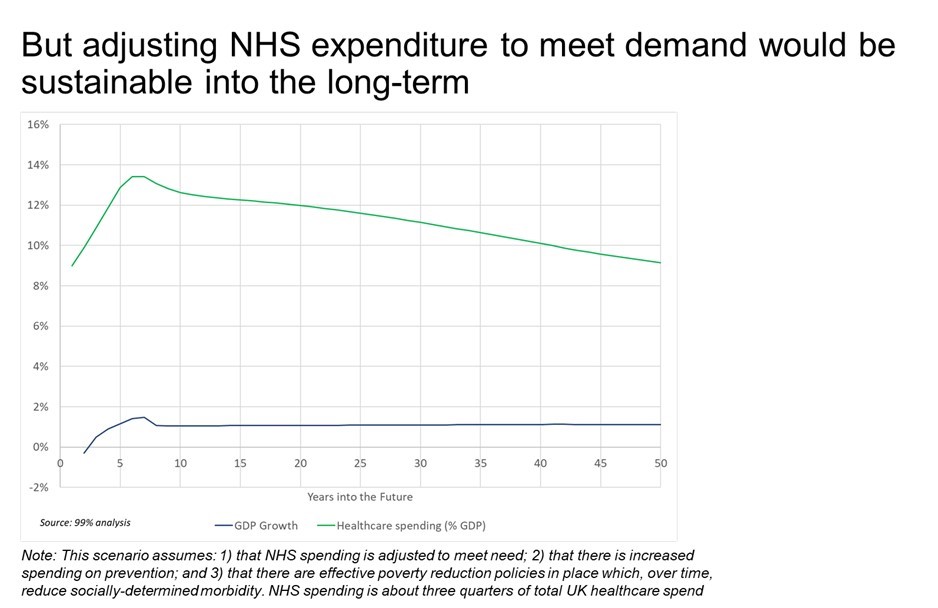
The analysis shows a short-term spike in spending as capacity is rebuilt, rather as we saw take place in the years 1997-2009, followed by a return to a steady state spending of around 9% of GDP. And the resulting GDP in the year 2060 would hit the OECD target.
Taking the message to Parliament
On 4 July, 2023, the team held a Parliamentary briefing, hosted by Richard Burgon, MP. Also present from Parliament were MPs: Caroline Lucas, Margaret Greenwood, Mary Kelly Foy, Kenny MacAskill, Ian Byrne, Micky Brady, Rachael Maskell, Liz Saville Roberts and Members of the House of Lords: Baroness Golding , Baroness Walmsley, and Lord Dubs.
The MPs and Peers received the reports findings enthusiastically and are planning to help the team to further the debate within Parliament by holding a Westminster Hall Debate, by introducing an Early Day Motion and by sharing the report with their front-bench colleagues.
The team is planning a similar event at Holyrood and, if possible, at the Welsh Assembly.
We aim to get the opposition parties to commit to the strategy set out above: 1) Fund the NHS properly; 2) increase spending on prevention; and 3) use GDP growth to fund effective poverty reduction measures. This will save both the NHS and the UK economy.
If you can help, let us know: https://99-percent.org/projects/helping-to-save-the-nhs/




